Introduction
SIL-TAL1 rearrangement is relatively common among patients with T-cell acute lymphoblastic leukemia (T-ALL). Pediatric patients with SIL-TL1 positive T-ALL generally have a poor response to early intensive treatment and a lower median relapse-free survival (RFS) and overall survival (OS) rates compared to pediatric T-ALL patients who do not harbor the SIL-TAL1 gene fusion. Therefore, we explored the clinical effect of haploid transplantation among pediatric SIL-TAL1-gene fusion positive T-ALL and aimed to identify potential patient prognostic factors.
Methods
We performed a retrospective analysis of 21 children with SIL-TAL1 gene fusion positive T-ALL who underwent haploidentical transplantation at the Lu Daopei Hospital in Langfang, China between July 2014 and June 2020. The median patient age was 9 years (range: 1.6 to 18 years), the male to female ratio was 19:2, and the median white blood cell count at initial onset was 193.65×109/L (range: 3.6-582.17×109/L). Prior to transplantation, 18 patients were bone marrow minimal residual disease (MRD) negative, three patients were bone marrow MRD-positive and the overall median value for MRD positivity by flow cytometry was 0.05% (range: 0.03%-0.35%). Eighteen patients were SIL-TAL1 gene fusion negative and three patients were SIL-TAL1 gene fusion positive prior to transplantation. The quantitative median number is 0.04% (range: 0.033%-0.05%). 13 patients with CR1 and 8 patients with CR2. 11 of 21 patients harbored the SIL-TAL1 gene fusion along with at least one other gene mutation. All patients were given myeloablative pretreatment, of which 17 patients received cyclophosphamide/total body irradiation (TBI/Cy) and 4 patients received Busulfan/cyclophosphamide (Bu/Cy). The median follow-up time was 9.5 months (range: 2 to 51 months).
Results
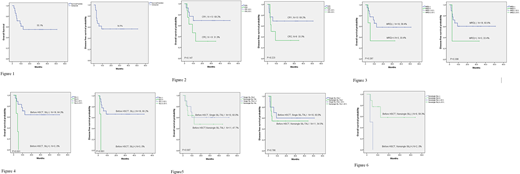
The white blood cells (WBCs) of 21 patients were all completely engrafted , two patients did not have platelet engraftment . At one month after transplantation, all patients were bone marrow MRD negative and the quantification of SIL-TAL1 fusion gene was 0% among all the patients. For 20 of these 21 patients, the chimerism rate of peripheral blood CD3+ cells and bone marrow was 100% donor type. The 4-year disease-free survival (DFS) and overall survival (OS) rate were 56.5% and 55.1%, respectively (Figure 1). Causes of death were recurrence (5 patients all of whom had bone marrow recurrence), infection (3 patients) and alveolar hemorrhage after reinfusion (1 patient). Six patients relapsed after transplantation with a median time to relapse of 90 days (range: 54-180 days). The OS rate following transplantation in the CR1 group was higher than in the CR2 groups (69.2% vs 31.3%, respectively) but there was no statistical difference between the two groups (P=0.147) (Figure 2). The OS rate of MRD-negative patients and MRD-positive patients prior to transplantation was 58.4% and 33.4% respectively, (P=0.287) (Figure 3). Prior to transplantation, the OS rate of SIL-TAL1 gene fusion-negative patients was 64.3%, while the OS rate of SIL-TAL1 gene fusion-positive patients was 0.0%--the difference between the two groups was statistically significant (P=0.001) (Figure 4). The OS rate of 11 patients that harbored the SIL-TAL1 gene fusion along with another gene mutation was 47.7% (Figure 5). Among these 11 patients, the OS rate of 9 patients who switched from SIL-TAL1 positive to SIL-TAL1 negative prior to transplantation was 58.3%. In contrast, two patients that remained SIL-TAL1 gene fusion positive had an OS rate of 0% (P=0.027) (Figure 6).
Conclusion
Pediatric T-ALL patients harboring the SIL-TAL1 gene fusion achieved a higher OS rate through haploid transplantation and were able to avoid extramedullary recurrence. We conclude that if patients with the SIL-TAL1 gene fusion do not switch to SIL-TAL1-negative prior to transplantation, we showed that even if the myeloablative pretreatment program is adopted, the survival rate cannot be improved, and the mortality rate is 100%. Harboring another gene mutation besides SIL-TAL1 at the initial onset of disease did not affect the prognosis in our cohort analysis. We conclude that for pediatric T-ALL patients, intensive chemotherapy should be adopted to make the bone marrow MRD negative and SIL-TAL1 gene fusion negative, and allogeneic hematopoietic stem cell transplantation should be performed as soon as possible to improve OS.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal